To the casual observer, the work comp bill review process is pretty simple:
- make sure the procedure codes are appropriate for the injury,
- compare the billed codes to the state fee schedule/allowable amount,
- apply any reimbursement rules, and you’re done.
The real story is far more complex. It’s no longer just about making sure the claim exists, the body part matches the medical report, and the procedure makes sense for the injury.
Reimbursement has gotten enormously complicated. Coding and code modifiers, bundled payment logic, clinical appropriateness, duplicate identification, relatedness, location of service verification, surgical groupers are just a few of the issues and considerations often unappreciated – and not considered – during the bill review process.
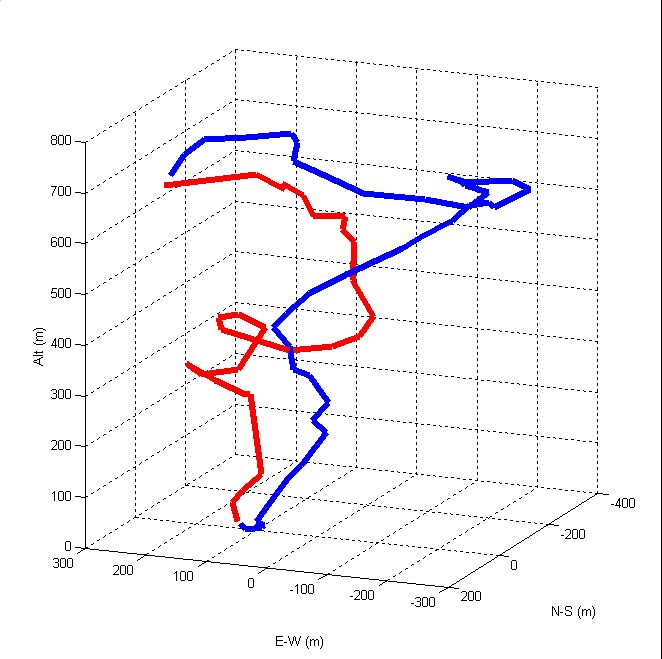
Far from A to B, it looks more like this – and is unique for some bills…
While some will say this is “not new news”, what is new is the constant focus and attention required to stay abreast of the ever-more creative and sophisticated “revenue maximization” industry. (That’s the label for provider-focused efforts to get as many payer dollars as possible)
I’ve taken a close look at several approaches/techniques intended to help payers keep pace with provider billing. One that caught my eye is Equian’s Clinical and Coding Logic. The folks at Equian were kind enough to spend a lot of time educating me on the research behind their Clinical & Coding Logic (CCL) solution, how it is used, and where it can have the most impact.
CCL has it’s roots in a commercial health application purchased by Equian some time ago, an application that has been adapted for use in workers’ comp. Building on that application, the company continues research to identify emerging billing practices, and develop identification techniques and rules to address those practices; to date more than 100 additional rules and millions of additional edits not found within typical bill review engines are in place.
There’s a LOT behind CCL; while I can’t provide more than a superficial overview, here’s a few things that popped up for me.
- Diagnosis and procedure codes with a “low-likelihood”of occurring in work comp are flagged; when they appear medical records are reviewed in detail
- Experimental and Investigational services typically fall thru the cracks in routine bill review processes; these have been identified and payment logic developed.
- CCL includes identification of services that appear to be body-part related but actually address pre-existing conditions
- Extensive research on the notorious 59 modifier enables reductions for inappropriate charges associated with surgery
Equally important is Equian’s ongoing research and analysis to identify emerging and previously unseen billing practices, development of identification techniques and rules, and evaluation of results.
CCL is a supplement to, not a substitute for the regular bill review process and technology. It requires data transmission to and from Equian via secure link, similar to PPO pend-and-transmit processes. Results shared by Equian demonstrate CCL is most useful for high-volume bill operations. Across the board, reductions average about $45 per bill (I was not able to independently verify savings or impact, and note that results are almost certainly highly contingent on each payer’s unique situation.)
What does this mean for you?
Never stand still.
Article source:Managed Care Matters
No comments:
Post a Comment